Buy discount feldene 20 mg online
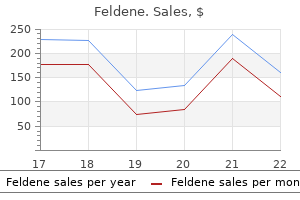
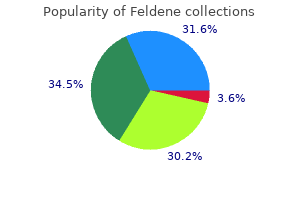
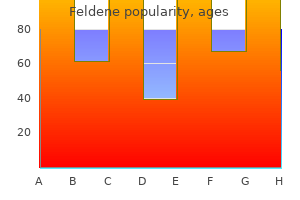
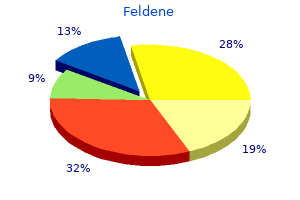
Much of the larger trochanter is apophyseal and forms the insertion for the hip abductors arthritis knee rain 20 mg feldene generic mastercard. Minimally displaced proximal femoral physeal separations have a better prognosis rheumatoid arthritis definition generic 20 mg feldene, very like these of an acute slipped capital femoral epiphysis. Intra-articular fractures of the femoral neck which are undisplaced may heal but also could displace. Extra-articular fractures of the femur (low neck, intertrochanteric, and subtrochanteric fractures) have a great prognosis for healing however tend to end in shortening, exterior rotation, and generally varus if untreated. There are progress plates beneath the capital femoral epiphysis, the greater trochanteric apophysis, and the lesser trochanteric apophysis. Femoral areas the place hips fracture: intracapsular neck (green), extracapsular neck (blue), and intertrochanteric�subtrochanteric space (red). Extra-articular fractures (low neck, intertrochanteric, and subtrochanteric fractures) in children lower than 6 years old could be handled by closed manipulation and spica casting. Preoperative Planning the injured hip ought to be evaluated under anesthesia using fluoroscopy. Approach Extra-articular fractures that are secure after reduction must be immobilized in a spica forged. Many neck fractures could be reduced closed and glued percutaneously from laterally. If the fracture could be anatomically reduced, the surgeon ought to proceed with percutaneous fixation; if not, open reduction should be undertaken. After reduction, pins are drilled from the lateral femoral cortex retrograde across the fracture. C D It is customary to use easy pins for physeal separations or neck fractures in very young children. A lateral view, often by frogging the hip, is critical to affirm pin placement. Because there may be a tense hemarthrosis that tamponades flow within the retinacular vessels of the neck, it might be clever to aspirate the joint capsule to evacuate or decompress the hip joint. The aim is anatomic discount to preserve perfusion to the capital femoral epiphysis, optimize bony apposition for healing, and forestall deformity, particularly varus and exterior rotation. The vastus lateralis is incised longitudinally, and the muscle tissue overlying the anterior hip capsule are elevated anteriorly. The incision is curved posteriorly after which extends distally in the posterior third of the vastus fascia. The angle the guidewire makes with the femoral shaft is dictated by the fixation device to be used. The fascia of vastus lateralis is "hockey sticked" and vastus muscle is retracted anteriorly, exposing the lateral femoral cortex. After fracture discount, a guidewire is inserted from the lateral femoral cortex up the femoral neck. The angle the wire makes with the lateral cortex ought to match the angle of the fixation system (usually one hundred thirty five degrees). Reaming is completed over the guidewire to accommodate the lag screw and the barrel of the aspect plate. The plate is secured to the femur with cortical screws and the compression screw locks the lag screw in the facet plate. The surgeon ought to contemplate decompressing the hemarthrosis to reduce the effect of tamponade of the vessels. Parents are warned in advance of the possibility and implications of avascular necrosis. Perfect discount and bony apposition present the best opportunity for fracture therapeutic. Decompression and stable inner fixation of femoral neck fractures in children can have an result on the end result. In youngsters who maintain a number of traumatic accidents, the nature and severity of each injury have to be thought of to optimize remedy. The proximal ossification middle is seen by 6 months and the distal femoral ossification middle seems at 7 months. The profunda femoris artery offers rise to 4 perforating arteries, which enter the femur posteromedially. During fracture healing, nonetheless, the majority of the blood is equipped by the periosteal circulation. The diploma of trauma required to trigger harm will increase exponentially as the character of the bone adjustments and progressively becomes stronger and larger from infancy to adolescence. Low-energy accidents leading to fractures might level to a pathologic nature of the condition, except in toddlers, in whom low-energy femur fractures are common. The place of the fracture fragments after the injury depends on the level of the fracture and displays the soft tissue and muscle forces appearing on the femur. In the setting of an isolated femur fracture, the thigh seems swollen with minor bruises and abrasions. Open wounds could change the management of this injury; apparent deformity helps within the preliminary analysis. The clinician palpates the length of the decrease extremity, feeling for bony deformity and checking compartments fastidiously for pressure. The clinicians ought to verify fastidiously for femoral, popliteal, dorsalis pedis, and posterior tibial pulses. Sensation to mild touch is tested along the length of the complete lower extremity. Diminished energy may indicate nerve harm or compartment syndrome or may also be secondary to pain. The clinician strikes the patellar and Achilles tendons with a reflex hammer and looks for contraction of the quadriceps and gastrocnemius, respectively. Diminished knee or ankle reflexes may indicate femoral or sciatic nerve damage or can also be secondary to guarding. In instances of high-energy trauma, concomitant injuries to the skin and soft tissue as properly as other organ techniques are usually present. Radiographs should include the joints above and below the fracture web site to keep away from missing any concomitant accidents. The clinician inspects the decrease extremity and looks for open wounds, bruising, or obvious deformity. For older youngsters and adolescents, three weeks of skeletal traction followed by spica casting was as quickly as frequent but has been changed by inner or external fixation generally. Preoperative Planning A detailed review of the clinical findings and all acceptable imaging studies is performed earlier than the procedure. Shortening ought to be decided to be less than 2 cm utilizing a lateral radiograph, although some counsel spica casting can be accomplished regardless of shortening.
Cheap 20 mg feldene visa
A pores and skin incision is revamped the anterolateral distal femur near rheumatoid arthritis age feldene 20 mg cheap overnight delivery the distal metaphysis arthritis knee swelling cheap 20 mg feldene with visa. The deep tissue is incised, and the vastus lateralis is elevated by blunt dissection to expose the lateral femoral cortex without disturbing the underlying periosteum. The osteotomy is carried out roughly 1 cm proximal to essentially the most proximal wire or half-pin attached to the distal ring. The cortex is drilled at the identical stage, with a number of drill holes at varying angles. A 5-mm osteotome is advanced via the anterior, lateral, medial, and posterior cortices. Square nuts or clickers are used with these connecting rods to permit for managed distraction. A completed femoral body with rings, connecting rods, wire/halfpins, and distal metaphyseal corticotomy. The quantity and site of wire/half-pin fixation, number of rings, and fundamental construct of the body are just like these described with the Ilizarov approach. Then the struts are disconnected and corticotomy is accomplished as mentioned earlier. The deformity, frame, and mounting parameters are entered within the software program, which prescribes a lengthening/deformity correction program. The femur and tibia frames had been linked with hinges to prevent knee subluxation during lengthening. Not really helpful for giant lengthening (more than 5 cm) the monolateral body is constructed earlier than the surgical procedure is finished. The design of the frame, including the number of clamps and arches, is dependent upon the deliberate lengthening. For easy lengthening (without deformity), three-point fixation is required in every phase. A guidewire is introduced parallel to the knee joint line and proximal to the expansion plate in children. Attach this half-pin to the clamp, which is related to the rail (monolateral fixator). At least one fingerbreadth of distance is maintained between the external frame and the lateral surface of the proximal thigh. On the lateral view, all the holes of the proximal and distal clamp ought to overlie the bone. The guidewire and half-pin are placed simply slightly anterior (not central) in the lateral femoral cortex. The proximal part of the distal clamp is approximately angulated by 10 to 15 degrees anteriorly. During femoral lengthening, delicate tissue tension predisposes the femur to develop procurvatum deformity. Procurvatum deformity could be prevented by making simple changes during frame utility. After the proximal half-pins have been positioned, the rail is disengaged from the proximal clamp. This pin placement creates a mild recurvatum deformity (10 degrees), which compensates for the anticipated procurvatum deformity. Gloves are changed, and the pores and skin on the stage of the corticotomy is prepped again. The femoral corticotomy is accomplished following the identical ideas discussed earlier. After completion of the corticotomy, the frame is reapplied, maintaining the same distance between the clamps and the skin. This recurvatum deformity compensates for the procurvatum tendency throughout lengthening of femur. Tibial Lengthening For easy lengthenings (without deformity), two- or three-point fixation is required in each bony phase. The tibial body usually includes a proximal clamp or arch with two or three half-pins and a distal fixation clamp with two or three half-pins. A distal tibia-fibula transfixation screw is required to forestall distal tibia-fibula subluxation. The pores and skin is incised over the tibial corticotomy website, which often is the proximal metaphysis. Prophylactic fasciotomy of the anterior compartment is carried out beneath direct vision before frame utility. Now a quick lived suture is positioned at the corticotomy skin incision, and corticotomy is performed after pin fixation is complete. The arch is placed parallel to the proximal tibial joint line, and the second half-pin is placed by way of the clamp. The anterior aspect of the arch should be at least a fingerbreadth from the anterior cortex. In the absence of deformity, the mechanical and anatomic axis of the tibia are the identical. Once again, parallel alignment of the body with the mechanical axis is confirmed. Gloves are modified, and the pores and skin on the stage of the proximal tibial metaphysis is prepared again. The frame is reapplied, sustaining the same distance between the clamps and the pores and skin as measured earlier than the corticotomy. The distraction gadget is related to the clamps, and last tightening is carried out. Confirm full osteotomy with fluoroscopy by externally rotating the distal fragment. Skeletal muscle relaxants may mask intraoperative nerve harm, and paralyzing agents are avoided. To prevent subluxation and dislocation of an adjacent joint throughout limb lengthening: Correct hip instability earlier than performing femur lengthening. Extend the frame across the knee joint within the setting of cruciate ligament laxity. Physical therapy to maintain range of motion and prevent contractures: Minimum: thrice a week, and a home program is performed 4 occasions a day During lively lengthening, the affected person is seen as soon as per week. They concluded that bigger lengthenings are potential, but the cost is increased time and complications. Pain with passive stretch and paresthesias are necessary medical signs of compartment syndrome. Prophylactic anterior compartment launch could additionally be performed at the time of corticotomy.
Feldene 20 mg without a prescription
Sequential broaching is then performed absorbine arthritis pain lotion feldene 20 mg low cost, with care to insert the broaches in appropriate anteversion arthritis in knee elderly buy feldene 20 mg without prescription. The degree of anteversion is greatest assessed visually if the assistant holds the tibia perpendicular to the plane of the ground. Sequential broaching is sustained till torsional stability is achieved at a depth of broach insertion that brings the proximal surface of the broach into the plane of the neck cut. If cautious preoperative templating was performed, this could lead to restoration of leg size and offset with the implant system being utilized. Many hip systems have choices for normal or prolonged offset necks; these may be defined by the amount of offset or by the neck�shaft angle. In basic, the neck that best recreated the anatomic geometry on preoperative templating should be chosen. If the coronal aircraft of the pelvis is perpendicular to the ground, the angle between the tibia and the ground is the mixed anteversion of the femoral and acetabular parts. The hip is internally rotated till the femoral head trial is coplanar with the rim of the acetabular part. Combined anteversion of 35 to forty five levels is perfect in girls, whereas somewhat less anteversion is desirable in males, who usually have much less lumbar lordosis. The anterior capsule must be free sufficient to permit external rotation of the femur such that the greater trochanter approaches one fingerbreadth away from the ischium, but not so loose as to enable impingement of the trochanter towards the ischium, or of the prosthetic neck towards the posterior socket. Third, the Steinmann pin is changed in the obturator foramen at the degree of the infracotyloid groove, and the relative lengthening or shortening of the leg is measured and noted. In basic, the objective is to increase the leg length by less than 5 mm to optimize hip stability without generating leg-length inequality. However this varies with preoperative scientific leg-length discrepancy and other components. The surgeon ought to feel a transparent delicate tissue resistance previous to dislocation, quite than a clean unimpeded movement. Some extra information may be gained from the Ober check, in which the knee is flexed ninety levels and the hip is extended to neutral and abducted. If the offset has been substantially increased, the knee will stay elevated (ie, the hip will remain abducted), indicating tightness of the iliotibial band. Results of this test are meaningless until compared to the preoperative findings, as some hips have a constructive Ober check preoperatively. A final test that provides extra restricted information is the "shuck" or "push-pull" take a look at, during which an assistant applies traction on the femur with the hip reduced however internally rotated, and the surgeon subjectively assesses the extent to which the femoral head may be distracted from the acetabulum. There should be some give with push-pull, however the assistant should be unable to completely dislocate the hip with easy traction. If the hip is discovered to be too loose, a plus-sized modular head can be utilized or the scale of the femoral stem could be increased such that the stem sits extra proudly within the femoral canal. If leg size is appropriate but offset is insufficient, the surgeon can switch from a regular to an extended-offset stem. If the anterior capsule is found to be tight in a hip with an otherwise acceptable reconstruction, we advocate anterior capsulotomy to stability the hip. If the hip is too tight-ie, with extreme anterior capsular tightness, a positive Ober take a look at, and excessive leglengthening-the femoral trial could be downsized or implanted deeper into the femur, or the minus-sized femoral head can be selected. We advocate in opposition to planning to use the minussized femoral head initially, because most implant methods have only a single minus measurement. Consequently, if the final reconstruction varies from the trial reconstruction, the surgeon is left without the choice of further reducing leg length and offset. This helps avoid unnecessarily long cement mantles which may be difficult to take away at revision, and it enhances cement pressurization. The femoral canal is then irrigated utilizing pulse lavage, dried using suction, and full of vaginal packing or a surgical sponge. Cement for the femoral side should be ready beneath vacuum or utilizing centrifugation, each of which improve cement energy by reducing cement porosity. Once the canal is crammed to the level of the neck minimize, the tip is removed from the cement gun and changed with a cement pressurizing device that occludes the proximal femoral canal. As pressurization is carried out, cement, fats, and marrow contents ought to be seen extruding from small vascular foramina in the femoral neck. When the pressurizer is removed from the femur, the void created must be full of extra cement. The surface of the cement is then dried with a sponge, and cement is used to coat the femoral stem, concentrating on the metaphyseal area. Both of those measures are meant to diminish the amount of blood, fluid, and other particles present within the cement and on the cement�prosthesis interface. If the femur has a comparatively broad diaphysis, the addition of a distal centralizer to the stem is suggested to scale back the risk of varus malpositioning. Pre-heating the stem will further cut back cement porosity and accelerate cement polymerization. Insertion is began by hand, impacting the insertion system with a mallet as needed. Once the position of the trial stem has been reproduced, light strain is maintained on the stem whereas excess cement is removed, and cement across the stem is pressurized by finger strain. Once the suitable head is chosen, the trunion of the stem is rigorously cleaned and dried, and the implant is gently impacted in place. The acetabulum is cleared of debris using irrigation and suction, and discount is carried out. The quadratus femoris is repaired to its insertion using nonabsorbable suture, together with restore of the gluteus maximus insertion if this tendon was released. Repair of the quick exterior rotators and posterior capsule to the posteromedial aspect of the larger trochanter is facilitated by two steps performed earlier in the case. These sutures usually are placed after acetabular cementing and before femoral preparation. During closure, the two sutures are handed through drill holes within the greater trochanter and tied to one another. To scale back working time, the drill holes are created whereas ready for the femoral cement to dry. Prior to tying the sutures, the leg is abducted and externally rotated, taking rigidity off the posterior delicate tissue flap being repaired to the larger trochanter. The restore must be inspected carefully to make positive that the posterior flap is in contact with the femur, quite than hanging by suture or sutures, earlier than the fascia is closed. The wound is once again copiously irrigated and routine closure of the fascia, subcutaneous tissue, and pores and skin is carried out. Patients with notably excessive offset must be warned that gentle lengthening of the leg may be essential to achieve acceptable soft tissue rigidity. However, small pores and skin incisions that limit publicity might place essential deeper constructions in danger for elevated trauma. Optimal cement fixation of the acetabular component is tough to achieve without a dry surgical subject, making hypotensive anesthesia a vital facet of cement method. Preoperative recombinant human erythropoietin could also be considered in sufferers unable to donate blood. Pain management Patient satisfaction is improved by the use of multimodal analgesia protocols,18 combining gentle tissue injections at the time of surgery, acetaminophen, nonsteroidal antiinflammatory medicines, and each long- and short-acting narcotics.
Feldene 20 mg generic amex
Clinical consequence of arthroscopic discount and suture for displaced acute and persistent tibial backbone fractures rheumatoid arthritis in dogs symptoms generic feldene 20 mg line. Comminuted tibial eminence anterior cruciate ligament avulsion fractures: failure of arthroscopic treatment rheumatoid arthritis disability feldene 20 mg line. Arthroscopic fixation of intercondylar eminence fractures utilizing a 4-portal approach. Tibial intercondylar fractures in children: a evaluate of the classification and the remedy of malunion. Arthroscopic fixation of avulsion fractures of the tibial eminence: method and end result. Magnetic resonance imaging aids in detecting concomitant accidents in patients with tibial spine fractures. Biomechanics of anterior cruciate ligament failure: an evaluation of strain-rate sensitivity and mechanisms of failure in primates. Pediatric and adolescent tibial eminence fractures: arthroscopic cannulated screw fixation. Tensile properties of the human femur-anterior cruciate ligament�tibia advanced: the effects of specimen age and orientation. Chapter 23 Anterior Cruciate Ligament Reconstruction in the Skeletally Immature Patient J. Conventional surgical reconstruction strategies danger potential iatrogenic progress disturbance due to physeal violation, and thus special consideration must be given to this affected person population. The ligament is composed of two anatomically and biomechanically distinct bundles, the anteromedial and the posterolateral bundles. It largely resists anterior translation and tightens within the final 30 levels of extension. Some have a tremendous quantity of progress remaining, while others are essentially accomplished growing. Most of the longitudinal progress of the decrease extremities comes from the distal femur and the proximal tibia. The posterior horn of the medial meniscus is a secondary restraint to anterior translation of the tibia. It is often due to a noncontact injury involving a cutting, pivoting, or fast deceleration maneuver. Physeal sparing reconstruction of the anterior cruciate ligament in skeletally immature prepubescent kids and adolescents: surgical method. Note increased sign on the posterior aspect of the lateral tibial plateau and the distal aspect of the femur at the sulcus terminalis (thick arrow). Complete tears in skeletally immature patients generally have a poor prognosis, with near-universal recurrent instability leading to further meniscal and chondral injury. Physiologic age must be established informally in the workplace using the Tanner staging system. Skeletal age may be determined through hand and wrist radiographs per the method of Greulich and Pyle. Particular consideration should be given to evaluating the knee for related pathology. Patella ballottement and fluid wave check ought to be accomplished to consider for the presence of an effusion. Loss of extension should alert the clinician to the potential of a displaced bucket-handle tear or preoperative arthrofibrosis. Tenderness to palpation must be assessed and localized particularly as it may possibly significantly direct the prognosis of associated accidents. Tenderness to palpation alongside the joint line, significantly the posterior aspect of the joint line, ought to alert the clinician to the potential for a meniscal tear. Pain or palpable popping with provocative maneuvers, corresponding to McMurray, Apley compression, or duck walk, will assist to verify this finding. Pain along the course of or at the femoral or tibial insertion points for the collateral ligaments ought to alert the clinician to the potential of a collateral ligament tear. Tenderness alongside the medial retinaculum or the course of the medial patellofemoral ligament can indicate an acute patellar dislocation that decreased spontaneously. Ligamentous evaluation ought to embody the anterior and posterior cruciate ligaments, the medial and lateral collateral ligaments, and the posterolateral nook. Skeletally immature athletes have a larger diploma of physiologic laxity than adult athletes, and as such a comparison should all the time be made to the uninjured knee. In the affected person who voluntarily or involuntarily guards towards traditional Lachman testing, the susceptible Lachman might encourage relaxation and give a more dependable examination. Pivot shift testing may be carried out in the workplace however is often not properly tolerated by pediatric patients. It should be performed within the operating room as part of the preoperative evaluation of every affected person. The posterior cruciate ligament should be evaluated using the posterior drawer check. The relative starting point ought to always be assessed first and compared to the contralateral aspect. Medial and lateral collateral ligament injuries are assessed by way of stress opening with valgus and varus stress at 0 and 30 levels of knee flexion. In the pediatric patient, opening with varus and valgus stress could be due to physeal accidents, and the clinician should at all times be vigilant for this. The posterolateral drawer and the exterior rotation recurvatum tests are additionally helpful for evaluating posterolateral corner injuries. Evaluation for patellar instability with apprehension testing ought to be performed. Evaluation of quadriceps bulk and energy is important for postoperative recovery. Special attention ought to be given to consider for physeal injuries in addition to different accidents on the differential diagnosis. Overall varus and valgus malalignment, if present clinically, should be evaluated with full-length, hip-to-ankle radiographs. This is likely as a result of the elevated vascularity of the meniscus, which is often interpreted as intrasubstance degeneration or a tear of the meniscus. For prepubescent sufferers with recurrent instability despite the above therapy, reconstruction is indicated. A tensioned delicate tissue graft in a bone tunnel throughout the physis can also induce a development disturbance. A number of reconstructive techniques have been used, including physeal-sparing, partial transphyseal, and transphyseal strategies utilizing various grafts. In prepubescent patients with giant amounts of progress potential remaining, we carry out a physeal-sparing, mixed intra-articular and extra-articular reconstruction utilizing autogenous iliotibial band. Recognizing that the physeal-sparing reconstruction described here is nonanatomic, we counsel patients and households that revision reconstruction could additionally be needed if recurrent instability develops, however that this procedure may temporize for additional growth such that the patient might then undergo a extra conventional reconstruction with drill holes. The following criteria have been shown to be related to successful nonoperative treatment of partial tears8: Tears of less than 50% of the ligament Relative preservation of the posterolateral bundle Age less than 14 years Normal or near-normal Lachman or pivot shift take a look at Up to a 3rd of patients could require subsequent reconstruction and should be made conscious of that threat on the onset of remedy.
Feldene 20 mg order with mastercard
Digital software program and templates to determine length and diameter of the nails can be found arthritis in the knee treatments best 20 mg feldene. Angular correction can also be estimated on digital radiographs arthritis in neck discs 20 mg feldene purchase with amex, but they can be deceiving due to the multiplanar nature of the angulation. The feminine nail could be reduce preoperatively, however I choose to cut the female nail intraoperatively, after the osteotomies are completed. The tibia is approached via a medial peripatellar incision, bluntly dissecting behind the patellar tendon when attainable without disrupting the synovium. If needed, an arthrotomy can be utilized to expose the beginning point for the tibial nail simply anterior to the tibial spines. The humerus is approached via a small deltoid-splitting incision to expose the higher tuberosity. A Positioning For fractures and deformities of the tibia and femur, the affected person is placed in the semilateral place with an axillary roll and a long, padded posterior roll close to the sting of the radiolucent table. Only one leg could be prepped at a time particularly if each the femur and tibia are being treated on the identical surgical setting. Ideally, the tip of the guidewire is positioned just medial to the center of the higher trochanter. It could also be difficult to visualize the larger trochanter in babies with poor bone density, and the insertion level could additionally be essentially in the piriformis fossa to avoid overreaming of the lateral cortex and to permit a straight line of advance to the femoral canal. Avascular necrosis has not been demonstrated in children in whom this technique has been used. An incomplete osteotomy is carried out whereas stability of the leg is maintained manually. The osteotomy is accomplished with light handbook stress, the guidewire is prolonged to the following osteotomy website, and the process is sustained till all deformities are corrected. Use of an extended guidewire may help to avoid capturing the guidewire within the reamer. Guidewire placed via the greater trochanter to the positioning of the primary osteotomy. Reaming can be done on the web site of the osteotomy to stabilize the proximal section. A 1-cm incision is revamped the apex of the osteotomy, and the gentle tissues are unfold to the periosteum. Gentle handbook traction and use of a lever such as a padded mallet will help to gently align and full the osteotomy site. The guidewire is eliminated to insert the male nail driver and nail after verifying the distal male nail thread size, while sustaining traction manually. Varus and valgus malalignment can be corrected with a distal osteotomy and correct placement of the nail within the center-center place in the distal femur. The threads are gently screwed into the epiphysis till the rounded portion of the rod positioned simply proximal to the threads is bridging the physis. The rod pusher is then positioned into the cannulated portion of the male nail driver, and a pointy backward blow is made on the T handle. The applicable size of the female nail is verified with the C-arm, as beforehand mentioned. The male nail driver is then removed, and the female nail is positioned over the male nail. The male nail is then inserted to the center-center position at the distal metaphysis. The female threads are shown simply barely partaking the bones of the greater trochanter to mitigate overgrowth of the trochanter. Distal placement of the male nail driver and nail in the center-center place is necessary. The threads interact the epiphysis of the distal femur, with the rounded, clean portion traversing the physis. Cutting the male nail roughly 1 cm above the highest of the female nail rarely causes persistent signs and allows for extra development. The probe is used to make positive that the cut male nail is clean and never bent, which might prevent telescoping. Occasionally, the diamond-tipped burr could also be necessary to easy the top of the male nail, however the soft tissues must be shielded from debris and damage. Revision When a rod system requires revision after maximal telescoping, it usually could be retrieved via just a proximal incision. A guidewire is positioned within the higher trochanter and into the cannulated portion of the female nail beneath fluoroscopic control. The male nail additionally may be retrieved with an arthroscopic alligator clamp after the female nail is eliminated. These have a somewhat shorter female-threaded portion to avoid extension of the threads throughout the proximal tibial epiphysis. Injury to the anterior horn of the medial meniscus is prevented with arthrotomy if necessary. With the knee kept flexed in extra of ninety levels, the guidewire is handed into the middle position of the proximal metaphysis and shaft. Typically, the wire tends to go posteriorly and laterally in order that the wire driver should be directed anteriorly and usually slightly medially. Alternatively, the wire may be manually pushed into the epiphysis if this offers higher control and visualization with the C-arm. The information pin could be advanced both with handbook pressure on the pin or utilizing a drill. While maintaining hip and knee flexion, the lateral radiograph may be carried out by merely abducting and externally rotating the leg. The guidewire is drilled down to the location of the first osteotomy, which regularly is the mid- to distal portion of the shaft of the tibia, though bowing of the proximal tibia also could also be current. When the medullary canal is obliterated by recurrent fracture and bowing, retrograde drilling is required to establish a medullary canal at the osteotomy website. Correct placement of the distal male nail after complete correction of anterolateral bowing. Closed osteoclysis of the fibula typically could be carried out with minimal pressure after the primary osteotomy, particularly in youthful kids, but open osteotomy may be necessary. The reamer is passed all the way down to the distal metaphysis while sustaining the knee in flexion at all times. Reaming ought to be accomplished slowly, with frequent stops on the apex of the angular deformity. Extending the knee whereas the reamer is in place can impinge and injure the femoral condyles. There is a small gap in the distal male nail to permit interlocking with a small wire, which is then bent over into the epiphysis. I have not used this system and have concerns about migration and retrieval of the wire with development.
Order 20 mg feldene overnight delivery
This toddler is comfy within the harness; hips and knees are flexed with abduction provided by gravity arthritis fingers playing guitar feldene 20 mg generic, not from the lateral straps arthritis symptoms in back or spine feldene 20 mg buy discount line. The anterior hip and lateral thigh incisions are usually parallel when the hip is flexed about 30 degrees. This is the deep fascia, which may then be further uncovered distally by utilizing a sponge on the fascia. If femoral shortening is anticipated, a separate direct lateral method to the proximal femur is used. Both exposures should be accomplished before osteotomies are performed due to increased bleeding from the bone. The fascia of the tensor muscle is entered barely lateral to the fatty interval between the 2 muscle tissue. Army-Navy retractors are used to separate the tensor and sartorius muscles until the rectus femoris muscle is recognized. This dissection is continued proximally and the prow of the pelvis is exposed between the anterior superior and anterior inferior iliac spines. The iliac crest apophysis is divided exactly within the center with a single reduce using a no. Laparotomy sponges are used to help dissect deep near the sciatic notch and to pack the surgical site for hemostasis. Perforating vessels into the iliac bone on the inside table are constantly current and require bone wax for hemostasis. Smooth Lane retractors are used to additional dissect the sciatic notch each medially and laterally. By opening the medial periosteum on the stage of the pubis, the iliopsoas tendon is recognized, which lies deep on the iliacus muscle. The tendon is adopted distally in order that the interval between the iliacus muscle and the rectus femoris muscle is separated more deeply. The iliopsoas tendon is introduced into the superficial surgical web site with a right-angled clamp and divided on the level of the iliopectineal groove on the pubis. The exterior oblique muscle has been detached off the iliac crest apophysis, which is being divided by a no. The iliopsoas tendon is identified, dissected distally, and divided at the iliopectineal eminence. Deep muscles of the iliacus, rectus femoris, and gluteus medius are mirrored off the hip capsule. The capsule have to be separated from any false acetabulum on the lateral iliac wall. The mirrored and straight heads of the rectus femoris muscle are recognized and divided. With a Kocher clamp, grasp the proximal facet of the mirrored head of the rectus femoris tendon to additional expose the capsule. The capsule have to be detached from the false acetabulum if present and uncovered superior and posterior. It is crucial to visualize the complete acetabulum and the transverse acetabular ligament. The ligamentum teres is removed with Mayo or cartilage scissors at its deep acetabular attachment. Under direct vision, a pituitary rongeur is used to take away the pulvinar tissue that lies inside the acetabulum. After any associated femoral and acetabular osteotomies are performed, the capsule is superior medially. For youngsters over 2�3 years of age, particularly if the reduction is tight or unstable, a femoral shortening osteotomy is carried out earlier than the capsule is closed. An adductor longus and gracilis tenotomy is generally not needed but could be included if these muscular tissues really feel excessively tight. The iliac crest apophysis is reapproximated with heavy suture and the exterior indirect muscle is reattached. A one-and-a-half spica forged is utilized with the hips in a safe "human" place with no more than 30 levels of flexion and abduction. The anterior edge of the gluteus medius muscle is recognized where it attaches to the higher trochanter. The vastus lateralis muscle ought to be divided off the posterior intermuscular septum so that the muscle innervation is left completely intact. Stiff Steinmann pins are inserted within the proximal and distal femur to make positive that a correct amount of femoral rotation is supplied. A third pin is placed up the neck of the femur to judge femoral head�neck antetorsion, and a fourth pin is positioned just below the lesser trochanter to guide the osteotomy. A subtrochanteric osteotomy is believed to be less hazardous to the hip vascularity than an intertrochanteric osteotomy. If extreme femoral torsion was noted, a few of this might be judiciously corrected. About 5 mm of probably the most anterior fringe of the gluteus medius muscle is detached from the larger trochanter in order that the femoral neck may be palpated and visualized (shown on a left hip). A one-third tubular plate has been attached to the proximal femur and a 2-cm section of bone has been removed from the subtrochanteric facet of the femur. The rigidity band of the vastus lateralis muscle is re-established with 0 absorbable suture. Bilateral hip dislocation could also be troublesome to decide as a outcome of the hips could additionally be symmetrically dislocated. An adolescent with newly identified hip dysplasia, particularly if bilateral, might have an underlying situation such as Charcot-Marie-Tooth illness. An insufficient closed discount or a reduction that requires excessive pressure or excessive place for stability can lead to osteonecrosis. Operative remedy In the anterior strategy, the surgeon ought to all the time acquire enough medial publicity and visualize the whole acetabulum. Femoral shortening is critical for a excessive dislocation if excessive force is required to deliver the femoral head into the joint. The older patient might have a simultaneous acetabular osteotomy for stability or due to extreme acetabular dysplasia. Patients older than 8 years with a dislocated hip, significantly those with bilateral dislocation, may have excessive deformity to justify reconstructive surgical procedure. Before starting treatment, the household must be cautioned about the risks of osteonecrosis and the chance of additional surgical procedure. Acetabular dysplasia after therapy for developmental dysplasia of the hip: implications for secondary procedures. Acetabular development after closed reduction of developmental dislocation of the hip. Closed reduction for congenital dysplasia of the hip: practical and radiographic results after a mean of thirty years.
Feldene 20 mg order line
Transverse orientation T12 pedicles are perpendicular to the floor within the transverse aircraft arthritis in the back exercises feldene 20 mg without a prescription. T1 pedicles subtend an angle of about 25 to 30 degrees with the midline in the transverse airplane arthritis fat fingers feldene 20 mg cheap otc. Thoracic pedicles progressively angle outward within the transverse aircraft, continuing superiorly from T12 to T1. This then transitions to a development toward a extra lateral and caudal pedicle starting point as one proceeds proximally from the apex. Lumbar Spine Anatomy the lumbar vertebral sides are more sagittally oriented compared to thoracic vertebral sides. Pedicles Dimensions In scoliotic spines, common lumbar pedicle length is 20 to 22 mm. The bigger measurement of the lumbar pedicles will increase the probability of optimal placement of pedicle screws. Transverse orientation L1 pedicles are perpendicular to the ground in the transverse airplane. L5 pedicles subtend an angle of about 25 to 30 levels with the midline in the transverse aircraft. Lumbar pedicles progressively angle outward within the transverse plane, continuing inferiorly from L1 to L5. The point of intersection for these two lines lies in the angle between the superior articular course of and the base of the transverse course of. Dangers Medial pedicular breaches endanger the dural sac, especially on the concavity of the curve. Inferior pedicular breaches endanger the nerve root, especially in the lumbar backbone. Advancement of pedicle screws following a lateral pedicular breach on the left can endanger the lung, segmental vessels, and sympathetic chain (T4�T12) and the aorta (T5�T10). Braces are unable to appropriate curves; their purpose is to prevent curve development. Advancement of pedicle screws following a lateral pedicular breach on the right can endanger the lung, segmental vessels, sympathetic chain, and azygous vein (T5�T11). Advancement of pedicle screws following a breach of the anterior cortex on the best can endanger the superior intercostal vessels (T4�T5), the esophagus (T4�T9), the azygous vein (T5�T11), the inferior vena cava (T11�T12), and the thoracic duct (T4�T12). Advancement of pedicle screws following a breach of the anterior cortex on the left can endanger the esophagus (T4�T9) and the aorta (T5�T12). With use of intraoperative fluoroscopic imaging guidance, data of anatomy stays crucial so as to orient the intensifier to obtain the most effective coronal pictures of the pedicles. Downgoing transverse process hook with upgoing pedicle hook on the same level or next-distal degree. Pedicle Screw Placement Advantages Pedicle screws have significantly greater axial pullout strengths than supralaminar hooks and pedicle hooks. Complications Suboptimal screw place More widespread in circumstances of severe deformity Perforation not uncommon (up to 40% of screws in some series) Lateral perforation extra common than medial perforation Lowest containment rates in midthoracic backbone (T5 to T8) Dural, neural, or vascular accidents happen sometimes. Types of pedicle screws Monoaxial No motion between the screw and the screw head Can acquire axial correction of deformity Uniaxial Motion between the screw and the screw head constrained to one aircraft Can accommodate sagittal contours whereas retaining capacity to get hold of axial correction (derotation) Polyaxial Multiaxial movement allowed between screw and screw head For lodging of sagittal contours Can accommodate malalignment of the starting factors within the coronal aircraft Reduction screw Pedicle screw with breakaway extended tabs Useful for seating rod into pedicle screw for tough reduction maneuvers Freehand placement of thoracic pedicle screws the easy trajectory allows for fixed-head screws and true direct vertebral derotation. Anatomic trajectory has an extended bone channel and permits an extended screw to be placed, but mandates the use of a multiaxial screw to join it to the rod. A easy trajectory paralleling the superior endplate has significantly higher pullout energy versus an anatomic trajectory that angles about 22 levels within the cephalocaudal direction perpendicular to the superior facet. Care must be given to the degree of hip flexion� extension, as this could affect the amount of lordosis in the lumbar spine. Care is taken to avoid abduction and forward flexion previous ninety levels on the shoulder and flexion previous 90 levels on the elbow. If a wake-up check is going to be used by the surgical staff, a transparent plastic C-arm cowl or equivalent clear drape is laid over the uncovered feet for visualization during the test. A disposable plastic ruler used for measuring the pedicle probe for pedicle depth is placed caudal to the sector on the buttocks and covered with a transparent Tegaderm dressing. Ideally, hooks must be placed flush with the bony surfaces to evenly distribute forces and decrease the prospect of hook pullout. This is accomplished by meticulous removing of the delicate tissues and even handed contouring of the bony surfaces: eradicating an extreme amount of bone can weaken hook buy, whereas removing too little bone can end result in improper seating of the hook. A vertical cut is made on the medial edge of the side, near the base of the spinous course of. A horizontal cut within the inferior aspect, allowing removing of three to 4 mm of bone, follows for insertion of the pedicle hook. To get hold of entrance into the canal, the ligamentum flavum is rigorously dissected from the laminae and utterly removed with curettes and rongeurs until the dura may be visualized. The costotransverse ligaments on the superior side of the transverse course of are divided with a periosteal elevator. Introduction of pedicle finder into facet joint, taking care to avoid canal penetration. Placement of a supralaminar hook is tough without bone removal to enable room for hook insertion. The surgeon must visualize the local topical anatomy and the effects of the scoliosis on the anatomy (rotation). The facet is osteotomized at the inferior border of the superior transverse process. Full publicity of the side joint facilitates identification of the place to begin. A cancellous blush usually heralds entry into the pedicle however could be a false optimistic found on entry into the transverse process. A specialized thoracic probe with a 2-mm blunt tip and a 35-mm curved phase with a rectangular cross part (Lenke probe) is used to create the tract for the pedicle screw. The probe is advanced using ventral strain and axial rotation to a depth of about 15 to 20 mm (the size of the pedicle), utilizing the suitable orientation for the particular vertebral degree (see Thoracic Pedicle Anatomy) and taking care to account for the scoliotic deformity. Typical twine lengths (distance from posterior cortical place to begin to anterior vertebral cortex according to the axis of the pedicle): Lower thoracic 40 to 45 mm Midthoracic 35 to forty mm Upper thoracic 30 to 35 mm the tract is probed using a versatile sound and 5 distinct bony borders are palpated: superior, inferior, medial, and lateral walls and the ground. The first 15 to 20 mm of the tract corresponds to the pedicle; its integrity must be critically assessed. After the cortex is breached, a curved probe is placed into the pedicle with the tip pointing laterally to decrease risk of medial pedicle breach and potential cord injury. After probing past the pedicle, its tip is then turned to point medially to decrease danger of vertebral body cortical breach. The facet joint is removed to obtain a flat surface before placing the pedicle screw. A specialized probe with a blunt spatula tip and a 35-mm curved section with a rectangular cross section (lumbar probe) is used to create the tract for the pedicle screw. The probe is launched into the beginning point with the curvature oriented so the tip is pointed laterally to avoid medial pedicle cortical violation.