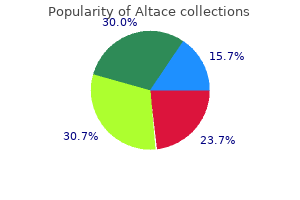
Cheap altace 10 mg on line
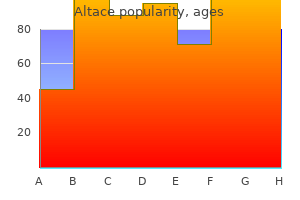
The mastoid element is fused with the descending means of the squamous part; below blood pressure record buy cheap altace 5 mg online, it seems within the posterior wall of the tympanic cavity blood pressure chart heart and stroke 2.5 mg altace quality. The posterior border, intermediate in length, bears a sulcus medially, which varieties, together with the occipital bone, a gutter for the inferior petrosal sinus. Behind this, the jugular fossa contributes (together with the occipital bone) to the jugular foramen and is notched by the glossopharyngeal nerve. Bone on either or either side of the jugular notch could meet the occipital bone and divide the jugular foramen into two or three components. The anterior border is joined laterally to the squamous part of the temporal bone at the petrosquamosal suture; medially, it articulates with the higher wing of the sphenoid bone. Two canals exist at the junction of the petrous and squamous components, one above the opposite, separated by a thin osseous plate and each leading to the tympanic cavity; the upper canal contains tensor tympani, whereas the lower canal is the pharyngotympanic tube. It is inclined superiorly and anteromedially, and has a base, apex, three surfaces (anterior, posterior and inferior) and three borders (superior, posterior and anterior). The base would correspond to the part that lies on the base of the skull and is separated from the squamous half by a suture. The subsequent development of the mastoid processes signifies that the precise boundaries of the bottom are not identifiable. The apex, blunt and irregular, is angled between the posterior border of the higher wing of the sphenoid and the basilar a half of the occipital bone. It accommodates the anterior opening of the carotid canal and limits the foramen lacerum posterolaterally. Bone anterolateral to this impression roofs the anterior a part of the carotid canal but is often deficient. A ridge separates the trigeminal impression from another hole behind, which partly roofs the interior acoustic meatus and cochlea. Laterally, the anterior floor roofs the vestibule and, partly, the facial canal. Between the squamous half laterally and the arcuate eminence and the hollows just described medially, the anterior surface is formed by the tegmen tympani, a skinny plate of bone that forms the roof of the mastoid antrum, and extends forwards above the tympanic cavity and the canal for tensor tympani. The lateral margin of the tegmen tympani meets the squamous part on the petrosquamosal suture, turning down in front because the lateral wall of the canal for tensor tympani and the osseous a half of the pharyngotympanic tube; its lower edge is within the squamotympanic fissure. Anteriorly, the tegmen bears a slender groove associated to the greater petrosal nerve (which passes posterolaterally to enter the bone by a hiatus anterior to the arcuate eminence). The posterior slope of the arcuate eminence overlies the posterior and lateral semicircular canals. Lateral to the eminence, the posterior a half of the tegmen tympani roofs the mastoid antrum. The posterior surface contributes to the anterior a half of the posterior cranial fossa and is steady with the inner floor of the mastoid part. A small slit leading to the vestibular aqueduct lies behind the opening of the meatus, almost hidden by a thin plate of bone. This contains the saccus and ductus endolymphaticus, together with a small artery and vein. The terminal half of the saccus endolymphaticus protrudes by way of the slit between the periosteum and dura mater. Near the apex of the petrous half, a quadrilateral area is partly associated with the attachment of levator veli palatini and the cartilaginous pharyngotympanic tube, and partly related to the basilar part of the occipital bone by dense fibrocartilage. Behind this region is the large, round opening of the carotid canal, and behind the opening of the canal is the jugular fossa, which is of variable depth and measurement, and contains the superior jugular bulb. The inferior ganglion of the glossopharyngeal nerve lies in a triangular melancholy anteromedial to the jugular fossa (below the inner acoustic meatus). At its apex is a small opening into the cochlear canaliculus, occupied by the perilymphatic duct (a tube of dura mater) and a vein draining from the cochlea to the interior jugular vein. A canaliculus for the tympanic nerve from the glossopharyngeal nerve lies on the ridge between the carotid canal and the jugular fossa. The mastoid canaliculus for the auricular branch of the vagus nerve is laterally positioned in the jugular fossa. Behind the jugular fossa, the tough quadrilateral jugular surface is roofed by cartilage that joins it to the jugular process of the occipital bone. Tympanic half the tympanic part of the temporal bone is a curved plate below the squamous half and anterior to the mastoid course of. Behind, it fuses with the squamous part and mastoid process, and is the anterior restrict of the tympanomastoid fissure. Its concave posterior surface types the anterior wall, flooring and a half of the posterior wall of the exterior acoustic meatus. The tympanic membrane is hooked up to a slender tympanic sulcus on its medial floor. The quadrilateral concave anterior surface is the posterior wall of the mandibular fossa and should contact the parotid gland. Its tough lateral border varieties a lot of the margin of the osseous a half of the external acoustic meatus and is steady with its cartilaginous part. Laterally, the upper border is fused with the back of the postglenoid tubercle; medially, it types the posterior edge of the petrotympanic fissure. The inferior border is sharp and splits laterally to form, at its root, the sheath of the styloid course of (vaginal process). The stylomastoid foramen lies between the styloid and mastoid processes; it represents the external finish of the facial canal, accommodates a half of the aponeurosis of the posterior stomach of digastric, and transmits the facial nerve and stylomastoid artery. Often virtually straight, it may possibly show a curvature, an anteromedial concavity being commonest. Its proximal half (tympanohyal) is ensheathed by the tympanic plate, particularly anterolaterally, while muscle tissue and ligaments are hooked up to its distal half (stylohyal). The styloid course of is roofed laterally by the parotid gland; the facial nerve crosses its base; the external carotid artery crosses its tip, embedded within the parotid; and medially, the process is separated from the start of the internal jugular vein by the attachment of stylopharyngeus. External acoustic meatus the temporal bone accommodates the bony (osseous) part of the exterior acoustic meatus. The squamous part is ossified in a sheet of condensed mesenchyme from a single centre close to the zygomatic roots, which seems in the seventh or eighth week in utero. The petromastoid half has a quantity of centres that seem in the cartilaginous otic capsule in the course of the fifth month; as many as 14 have been described. Key: 1, helix; 2, crus of helix; 3, auricular tubercle; 4, antihelix; 5, crura of antihelix; 6, triangular fossa; 7, scaphoid fossa; 8, concha of auricle; 9, external acoustic meatus; 10, tragus; eleven, antitragus; 12, intertragic notch; 13, lobule of auricle. The styloid process develops from two centres at the cranial finish of cartilage within the second visceral or hyoid arch; a proximal centre for the tympanohyal appears before birth, and another, for the distal stylohyal, appears after birth. The tympanic ring unites with the squamous half shortly earlier than delivery, and the petromastoid fuses with it and the tympanohyal during the first year. Once ossified, the tympanic cavity, mastoid antrum and the posterior end of the pharyngotympanic tube turn out to be surrounded by bone.
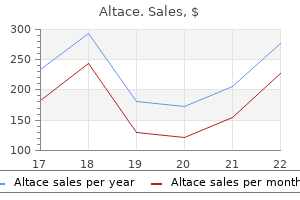
Altace 2.5 mg cheap line
Medial to the ligament heart attack cover by sam tsui and chrissy costanza of atc order 5 mg altace amex, each medial department sends articular branches to the facet joints above and below its course pulse pressure emedicine altace 10 mg otc, before getting into multifidus, which it supplies. It communicates with the fourth and fifth sacral dorsal rami to supply the pores and skin over the coccyx. Three main longitudinal vessels, a single anterior and two posterior spinal arteries (each of which is sometimes doubled to cross on either side of the dorsal rootlets) originate intracranially from the vertebral artery and terminate in a plexus across the conus medullaris. The anterior spinal artery forms from the fused anterior spinal branches of the vertebral artery, and descends within the ventral median fissure of the cord. Each posterior spinal artery originates either immediately from the ipsilateral vertebral artery or from its posterior inferior cerebellar department, and descends in a posterolateral sulcus of the cord. The segmental arteries are derived in craniocaudal sequence from spinal branches of the vertebral, deep cervical, intercostal and lumbar arteries. These vessels enter the vertebral canal by way of the intervertebral foramina and anastomose with branches of the longitudinal vessels to type a pial plexus on the surface of the wire. The segmental spinal arteries ship anterior and posterior radicular branches to the spinal twine along the ventral and dorsal roots. Most anterior radicular arteries are small and end in the ventral nerve roots or in the pial plexus of the wire. The small posterior radicular arteries additionally provide the dorsal root ganglia; branches enter at both ganglionic poles to be distributed round ganglion cells and nerve fibres. The anterior longitudinal artery and the intramedullary arteries are practical end-arteries, although overlap of territories of supply has been described (Backes and Nijenhuis 2008). This is very true of the artery of Adamkiewicz, which can effectively carry the main supply for the lower wire; injury to this individual artery compromises perfusion of the distal twine and could also be responsible for paraplegia following aortic bypass procedures. For a few years, it was assumed that the anterior spinal artery system supplied the dominant supply to the twine, but clinical proof implies that the posterior spinal arteries could also be as important as the anterior system in defending the wire. The mid-thoracic twine, distant from the primary anterior medullary feeders, is particularly liable to turn out to be ischaemic after durations of hypotension; T4�9 has been described because the crucial vascular zone of the spinal twine, the place interference with the circulation is most probably to result in paraplegia. Only the anterior spinal vein, which drains the central grey matter, is constantly full. It receives sulcal veins and small pial veins from the coronal plexus and is largest in calibre within the lumbosacral region. The posterior spinal vein is frequently variable, appearing plexiform in some segments and as a single channel in others. These vessels connect freely and drain superiorly into the cerebellar veins and cranial sinuses, and segmentally into medullary veins mainly. Segmental radiculomedullary feeder arteries Some radicular arteries, primarily situated within the decrease cervical, decrease thoracic and upper lumbar regions, are giant enough to reach the ventral median fissure, where they divide into slender ascending and large descending branches. They anastomose with the anterior spinal arteries to kind a single or partly double longitudinal vessel of uneven calibre alongside the ventral median fissure. The largest anterior medullary feeder, the good anterior radiculomedullary artery of Adamkiewicz, varies in degree, arising from a spinal department of either one of many lower posterior intercostal arteries (T9�11), or of the subcostal artery (T12), or less frequently of the upper lumbar arteries (L1 and L2). Reaching the spinal wire, it sends a department to the anterior spinal artery below and another to anastomose with the ramus of the posterior spinal artery, which lies anterior to the dorsal roots. Each posterior spinal artery contributes to a pair of longitudinal anastomotic channels, anterior and posterior to the dorsal spinal roots. These are strengthened by posterior medullary feeders from the posterior radicular arteries. The latter are variable in number and size, but smaller, more numerous and extra evenly distributed than the anterior medullary feeders. The anterior channel is joined by a ramus from the descending branch of the nice anterior segmental medullary artery of Adamkiewicz. In all longitudinal spinal arteries the width of the lumen is uneven and complete interruptions could occur. Anastomoses apart from those between the pial or peripheral spinal arterial branches could additionally be essential. Very small anterior and posterior radicular veins happen in most spinal segments, accompanying and draining the ventral and dorsal roots and a few of the wire on the points of entry and exit of the rootlets; they often drain into the intervertebral veins. The remainder of the dorsal gray and white columns and peripheral parts of the lateral and ventral white columns are supplied by quite a few small radial vessels that branch from posterior spinal arteries and the pial plexus. In a microangiographic examine of the human cervical spinal twine, up to six anterior, and eight posterior, radicular spinal arteries were described, and as much as eight central branches arose from every centimetre of the anterior spinal artery (Turnbull et al 1966). B, the adjustments have been famous to be in the distribution of the anterior spinal artery, as seen on this axial image. In estimating the vertebral levels of cord segments within the adult, a useful approximation is that, within the cervical region, the tip of a vertebral spinous course of corresponds to the succeeding twine phase. The eleventh thoracic spine overlies the third lumbar section and the twelfth is opposite the first sacral phase. In making this estimate by palpation of the vertebral spines, it is very important bear in mind the connection of the individual spines to their vertebral bodies. Clinical localization may be off by a number of ranges because different factors could come into play, corresponding to vascular insufficiency or venous obstruction, ensuing in the lesion being localized as significantly lower than it really is (Rousseff and Tzvetanov 2006, Sonstein et al 1996). Complete division above the fourth cervical segment causes respiratory failure because of the lack of activity within the phrenic and intercostal nerves. Lesions between C5 and T1 paralyse all 4 limbs (quadriplegia), the effects within the higher limbs various with the positioning of damage: on the fifth cervical section, paralysis is full; and at the sixth, each arm is positioned in abduction and lateral rotation, with the elbow flexed and the forearm supinated, due to unopposed activity in deltoid, supraspinatus, rhomboid and the brachial flexors (all provided by the fifth cervical spinal nerves). However, sensation is retained in areas innervated by segments above the lesion; thus cutaneous sensation is retained within the neck and chest right down to the second intercostal house because this area is innervated by the supraclavicular nerves (C3 and C4). At thoracic ranges, division of the cord paralyses the trunk under the segmental level of the lesion, and each lower limbs (paraplegia). The first sacral neural segment is approximately degree with the thoracolumbar vertebral junction; harm, which commonly happens right here, paralyses the urinary bladder, the rectum and muscle tissue equipped by the sacral segments, and cutaneous sensibility is lost within the perineum, buttocks, the again of the thighs and the legs, and soles of the ft. The roots of lumbar nerves descending to be a part of the cauda equina could also be damaged at this stage, inflicting complete paralysis of both lower limbs. Lesions below the primary lumbar vertebra might divide or damage the cauda equina, but severe nerve injury is unusual and is often confined to the spinal roots on the stage of the trauma. Neurological symptoms may also happen as a outcome of interference with the spinal blood provide, particularly within the lower thoracic and upper lumbar segments. This mostly happens with motorcar accidents but in addition has been reported with sports activities accidents and falls. Neurofibromas and schwannomas may occur on the roots and nerves within the root canals. As they enlarge, these tumours turn into dumbbell-shaped, with each an intraspinal and an extraspinal component in continuity; the scientific image might thus embrace paradoxical features because the asymmetrical space-occupying lesion grows. Root compression often presents Spinal cord and spinal nerves: gross anatomy Typical neural abnormalities embrace cord oedema, haemorrhage, contusion or transection.
Generic altace 2.5 mg on line
The third half is the arteria profunda linguae blood pressure chart 2015 purchase 10 mg altace amex, which turns upwards near the anterior border of hyoglossus after which passes forwards close to blood pressure chart software free buy altace 2.5 mg on-line the inferior lingual floor close to the frenulum, accompanied by the lingual nerve. Genioglossus is a medial relation, and the inferior longitudinal muscle of the tongue lies lateral to it beneath the lingual mucous membrane. Near the tip of the tongue, the lingual artery anastomoses with its fellow of the alternative aspect. Occipital artery Suprahyoid artery the suprahyoid artery is a small department that runs along the higher border of the hyoid bone to anastomose with the contralateral artery. Dorsal lingual arteries Sublingual artery Facial artery the dorsal lingual arteries are described on web page 513. At first on the middle pharyngeal constrictor, it might reach the lateral floor of styloglossus, separated there from the palatine tonsil solely by this muscle and the lingual fibres of the superior constric tor. Medial to the mandibular ramus, it arches upwards and grooves the posterior aspect of the submandibular gland. It then turns down and descends to the decrease border of the mandible in a lateral groove on the submandibular gland, between the gland and medial pterygoid. Reach ing the floor of the mandible, the facial artery curves round its inferior border, anterior to masseter, to enter the face; its further course is described on web page 498. In the neck, this may be in order that the artery is ready to adapt to the move ments of the pharynx during deglutition, and equally on the face, in order that the artery can adapt to movements of the mandible, lips and cheeks. Facial artery pulsation is most palpable the place the artery crosses the mandibular base, and once more close to the nook of the mouth. Its branches in the neck are the ascending palatine, tonsillar, submental and glandular arteries. At its origin, the artery is crossed superficially by the hypoglossal nerve, which winds spherical it from behind. The artery subsequent passes backwards, up and deep to the posterior belly of digastric, and crosses the inner carotid artery, internal jugular vein, and hypoglossal, vagus and accent nerves. Between the transverse means of the atlas and the mastoid course of, the occipital artery reaches the lateral border of rectus capitis lateralis. It then runs in the occipital groove of the temporal bone, medial to the mastoid process and attachments of sternocleidomastoid, splenius capitis, longissimus capitis and digastric, and lies successively on rectus capitis lateralis, obliquus superior and semispinalis capitis. The occipital artery has two major branches (upper and lower) to the upper a half of sternocleidomastoid within the neck. The lower branch arises near the origin of the occipital artery, and may typically arise directly from the exterior carotid artery. It descends backwards over the hypoglossal nerve and inside jugular vein, enters sternocleidomastoid and anastomoses with the sternocleidomastoid branch of the superior thyroid artery. The upper department arises because the occipital artery crosses the accessory nerve, and runs down and backwards superficial to the intern al jugular vein. Posterior auricular artery 454 the posterior auricular artery is a small vessel that branches posteriorly from the external carotid just above digastric and stylohyoid. It ascends between the parotid gland and the styloid course of to the groove between the auricular cartilage and mastoid process, and divides into auricular and occipital branches, that are described with the face on page 499. In the neck, it offers branches to provide digastric, stylohyoid, sterno cleidomastoid and the parotid gland. It also offers origin to the stylo mastoid artery � described as an oblique branch of the posterior auricular artery in a few third of subjects � which enters the stylo mastoid foramen to supply the facial nerve, tympanic cavity, mastoid antrum air cells and semicircular canals. In the younger, its posterior tympanic ramus forms a circular anastomosis with the anterior tym panic branch of the maxillary artery. The length of the artery varies with the length of the neck and the point of the carotid bifurcation. It may come up from the aortic arch, by which case it lies medial to the external carotid so far as the larynx, where it crosses behind it. The cervical portion is generally straight however could additionally be very tortuous, when it lies nearer to the pharynx than usual, very near the tonsil. In youngsters, the tonsillocarotid distance will increase with growth to a maximum value of 25 mm (Deutsch et al 1995). Carotid sinus and carotid physique Internal carotid artery the interior carotid artery provides many of the ipsilateral cerebral hemisphere, eye and accent organs, brow and, in part, the nose. Here, it enters the cranial cavity and turns anteriorly by way of the cavern ous sinus within the carotid groove on the facet of the physique of the sphenoid bone. It terminates under the anterior perforated substance by division into the anterior and middle cerebral arteries. It may be divided con veniently into cervical, petrous, cavernous and cerebral components. Rarely, persistent embryonic branches to the basilar artery from the cervical a part of the inner carotid artery may be encountered at the C1�C2 (persistent hypoglossal artery) and C2�C3 (proatlantal intersegmental artery) levels. Relations the internal carotid artery is initially superficial within the carotid triangle, after which passes deeper, medial to the posterior belly of digastric. Except close to the cranium, the inner jugular vein and vagus nerve are lateral to it throughout the carotid sheath. The exterior carotid artery is first anteromedial, but then curves again to lie superficial. Pos teriorly, the inner carotid adjoins longus capitis, and the superior cervical sympathetic ganglion lies between them. The pharyngeal wall lies medial to the artery, which is separated by fat and pharyngeal veins from the ascending pharyngeal artery and superior laryngeal nerve. Below the posterior stomach of digastric, the hypoglossal nerve and superior root of the ansa cervicalis and the lingual and facial veins are superficial to the artery. At the level of the digastric, the inner carotid is crossed by stylohyoid and the occipital and posterior auricular arteries. At the base of the cranium, the glossopharyngeal, vagus, the widespread carotid artery has two specialised organs near its bifur cation: the carotid sinus and the carotid body. They relay info in regards to the stress and chemical composition of the arterial blood, respectively, and are innervated principally by the carotid branch(es) of the glossopharyngeal nerve, with small contributions from the cervical sympathetic trunk and the vagus nerve. The carotid sinus often appears as a dilation of the decrease end of the inner carotid in late adolescence (Seong et al 2005) and functions as a baroreceptor. It lies either posterior to the carotid bifurcation or between its branches, and is connected to , or generally partly embedded in, their adventitia. Aberrant miniature carotid our bodies, micro structurally related however with diameters of 600 �m or much less, could appear in the adventitia and adipose tissue close to the carotid sinus. The carotid body is surrounded by a fibrous capsule, from which septa divide the enclosed tissue into lobules. Unmyelinated axons lie in a collagenous matrix between the sustentacular cells and the sinusoidal endothelium, and many synapse on the glomus cells. They are visceral afferents, which journey in the carotid sinus nerve to join the glossopharyngeal nerve. Preganglionic sympathetic axons and fibres from the carotid sinus synapse on para sympathetic and sympathetic ganglion cells, which lie both in isola tion or in small teams close to the floor of every carotid body. Postganglionic axons journey to local blood vessels; the parasympathetic efferent fibres are in all probability vasodilatory and the sympathetic ones are vasoconstrictor.
Buy discount altace 10 mg line
Usually arrhythmia medications cheap 10 mg altace with visa, patients with this situation have a cutaneous abnormality arrhythmia questionnaire 2.5 mg altace purchase fast delivery, such as a dimple, pigmented naevus or patch of hair, along their again at the stage of the tethering. At later phases, satellite cells originating from the dermomyotome enter the myotome. The mechanism of growth of endo-, peri- and epimysium in relation to the epaxial muscular tissues has not been conclusively determined. At cervical and trunk ranges, myotubes are produced by the ventrolateral fringe of the dermomyotome in a manner just like the manufacturing of epaxial muscle tissue. As growth proceeds, lateral development of the dermomyotome signifies that the ventrolateral border extends ventrolaterally into the developing lateral and ventral body wall. This process has been shown to rely upon the homeoboxcontaining transcription factor Pitx2 (Eng et al 2012). The somite structures that invade the somatopleure of the belly and thoracic partitions thus consist of two layers, dermomyotome and myotome, that give rise to the muscle blastemata for the intercostal and oblique muscles, transversus abdominis and rectus abdominis. At this time, the variety of somatopleural fibroblasts situated inside the muscle-forming zone will increase, and myotubes may be first seen. There is a subsequent ventral shift of the already separated muscle blastemata inside the growing abdominal wall as they attain their definitive positions. Muscle differentiation continues and muscular connective tissue, tendons and aponeuroses develop. Myoblasts transfer from the occipital dermomyotomes into the growing mandibular processes to form the intrinsic muscle tissue of the tongue, whereas those opposite the early limb buds migrate into the limbs as dorsal and ventral muscle masses that give rise to the shoulder, hip and appendicular muscle tissue. Longitudinal scans of the fetal backbone can demonstrate scoliosis and hemivertebrae. Anomalies of the spine (spina bifida) are among the many most common fetal malformations noted on antenatal ultrasound examination. The Northern Congenital Abnormality Survey reported a total prevalence at delivery and termination of 17. Muscles within the head come up from the unsegmented paraxial mesoderm rostral to the occipital somites. The dorsomedial lip (border) of the dermomyotome is an infolding of the epithelial plate of the somite and turns into a proliferative epithelial website from which mediolateral progress of the dermomyotome itself happens. Three constructions are required for myogenesis: the neural tube, the notochord/neural ground plate complicated and the (early) dorsally positioned ectoderm. There is a stability between ranges of Shh from the notochord and Wnts from the dorsal neural tube and ectoderm, which promotes myogenesis; high ranges of either alone lead to sclerotomal or non-myogenic dermomyotomal development (Scaal and Christ 2004). In this model, all four borders of the dermomyotome give rise to myotomal cells, produced in two phases. First, cells are produced from the dorsomedial dermomyotomal lip by direct ingression and bidirectional extension. Second, myotomal precursor cells are released by the caudal dermomyotomal border, followed, in flip, by the cranial dermomyotomal border, and lastly, by the ventrolateral dermomyotomal lip. Those myotomal cells arising from the dorsomedial dermomyotomal border contribute cells exclusively to the epaxial area, whereas these from the ventrolateral border contribute cells completely to the hypaxial area. Later in improvement, proliferative muscle progenitor cells originating from the de-epithelializing dermomyotome contribute to fetal muscle development (Gros et al 2005). The cells endure an epithelial/mesenchyme transformation from the dermomyotome and migrate to the dorsomedial subectodermal space overlying the dorsal neural tube. Somitic cells are actually thought-about to give rise to clean muscle cells inside and across the growing somites, and within the tunica media of the descending aorta (Wiegreffe et al 2007). All compartments of the epithelial somite, including the somitocoele cells, give rise to angioblasts. The early ventral half of the somite provides rise to the endothelium of ventrolateral blood vessels. Angioblastic cells arising from the dorsomedial dermomyotome migrate mainly into the dorsal dermis, whereas these arising from the dorsolateral part transfer to the ventrolateral physique wall and limbs (Scaal and Christ 2004). Lower panel: three-dimensional ultrasound floor rendering mode exhibits the spinal defect in the sagittal (A and B) and coronal (C) views. Early myotome cells are postmitotic embryonic myoblasts; later in growth, they fuse to form syncytia, which produce the intrinsic muscular tissues of the again. This paper presents first and early second trimester growth of bones, joints and ligaments of the craniovertebral junction. This paper clearly demonstrates the craniocervical junction in staged human embryos. An overview of the development of the dorsal somite compartment to dermis and muscle. Christ B, Huang R, Scaal M 2004 Formation and differentiation of the avian sclerotome. Gros J, Scaal M, Marcelle C 2004 A two-step mechanism for myotome formation in chick. Gros J, Manceau M, Thom� V et al 2005 A common somitic origin for embryonic muscle progenitors and satellite tv for pc cells. Hita-Contreras F, Roda O, Mart�nez-Amat A et al 2014 Embryonic and early fetal period development and morphogenesis of human craniovertebral junction. Huang R, Zhi Q, Brand-Saberi B et al 2000 New experimental evidence for somite resegmentation. Muhleman M, Charran O, Matusz P et al 2012 the proatlas: a comprehensive evaluation with medical implications. A presentation of three completely different fashions of somite formation in the context of molecular data. Wiegreffe C, Christ B, Huang R et al 2007 Sclerotomal origin of smooth muscle cells in the wall of the avian dorsal aorta. The cervical enlargement, the source of the large spinal nerves that provide the higher limbs, extends from the third cervical to the second thoracic segments. Its maximum circumference (approximately 38 mm) is in the sixth cervical segment (a spinal cord segment offers the attachment of the rootlets of a pair of spinal nerves). The lumbar enlargement, the supply of the large spinal nerves that provide the lower limbs, extends from the primary lumbar to the third sacral segments; the equivalent vertebral levels are the ninth to twelfth thoracic vertebrae. Its greatest circumference (approximately 35 mm) is close to the lower part of the physique of the twelfth thoracic vertebra, below which it rapidly dwindles into the conus medullaris. Perforating branches of the spinal vessels move from the fissure to the commissure to provide the central spinal area. The posterior median sulcus is shallower, and from it a posterior median septum penetrates more than halfway into the wire, almost to the central canal. The septum varies in anteroposterior extent from four to 6 mm, and diminishes caudally as the canal turns into more dorsally positioned and the twine contracts.
Cheap altace 2.5 mg visa
Acute inflam mation of the parotid gland (acute sialadenitis) might cause exquisite pain in the preauricular area because of stretching of the capsule and stimulation of the good auricular nerve arteriovenous graft generic altace 2.5 mg online. The pain is often exacer bated at mealtimes when the gustatory stimulus to the gland ends in further turgor inside the capsule blood pressure medication ringing in ears altace 10 mg buy cheap line. Causes of acute sialadenitis embrace parotid duct obstruction (calculus, mucus plug and duct stricture) and mumps. It crosses masseter, turns medially at its anterior border at nearly a right angle, and traverses the buccal fat pad and buccinator opposite the crown of the upper third molar tooth. The duct then runs obliquely forwards for a short distance between buccinator and the oral mucosa earlier than it opens on a small papilla reverse the second upper molar crown. The submucosal passage of the duct serves as a valvular mechanism, stopping inflation of the gland with raised intraoral pressures. While crossing masseter, the duct lies between the upper and decrease buccal branches of the facial nerve, and may obtain the accent parotid duct. The accent part of the gland (Fromer 1977) and the transverse facial artery lie above the parotid duct; the buccal branch of the man dibular nerve, rising from beneath temporalis and masseter, lies just below, on the anterior border of masseter. The parotid duct may be crossed by anastomosing branches between the zygomatic and buccal branches of the facial nerve. The ramifications of the ductal techniques, and their patterns and cali bres, could be demonstrated radiographically by injecting a radioopaque substance into the parotid duct by way of a cannula. In a lateral parotid sialo gram, the primary duct can be seen to be shaped close to the centre of the posterior border of the mandibular ramus by the union of two or three ducts that ascend or descend, respectively, at proper angles to the primary duct. Deep lacerations of the cheek, where the integrity of the parotid duct is doubtful, ought to be explored and repaired using microsurgical techniques, to stop saliva leaking into the delicate tissues of the cheek and subsequent sialocele formation. Lymph nodes happen in the skin overlying the parotid gland (pre auricular nodes) and in the substance of the gland. There are usually ten lymph nodes current in the gland; the bulk lie within the superficial part of the gland above the plane related to the facial nerve. Postganglionic secretomotor fibres reach the gland via the auriculotemporal nerve. It is thought to reflect aberrant innervation of sweat glands on the face by regrowing parasympathetic secretomotor axons that would beforehand have innervated the parotid gland. Denerv ation by tympanic neurectomy or auriculotemporal nerve avulsion has been advocated but is usually not healing. The symptoms may be managed by the subcutaneous infiltration of purified botulinum toxin into the affected area and use of antiperspirant. Note that right here the main duct is shaped by the union of three smaller ducts at the posterior border of the ramus of the mandible. B, In this case, the intact proper medial wall (green line) was mirrored; the pink line outlines the defect on the left orbit. The contribution of anatomy to the pathogenesis of floor and medial orbital fractures is elegantly shown. An old paper however the method described is a very practical application of exploiting the anatomy of the temporal fossa. A detailed account of the procedures for the protected dissection of the intraparotid a part of the facial nerve. The flooring of the mouth is fashioned by the mylohyoid muscles and is occupied primarily by the tongue. Three pairs of main salivary glands (parotid, submandibular and sublingual) and quite a few minor salivary glands (labial, buccal, palatal, lingual) open into the mouth. The muscular tissues in the oral cavity are related to the lips, cheeks, flooring of the mouth and tongue. The muscle tissue of the taste bud are described with the pharynx in Chapter 34 (Berkovitz and Moxham 2002). The mouth is anxious primarily with the ingestion and masti cation of food, which is especially the perform of the enamel. The parotid duct drains into the cheek opposite the maxillary second molar tooth at a small parotid papilla. A hyperkeratinized line (the linea alba) may be seen at a posi tion associated to the occlusal aircraft of the teeth. In the retromolar area, a fold of mucosa containing the pterygomandibular raphe extends from the upper to the lower alveolus. The entrance to the pterygomandibular space (which incorporates the lingual and inferior alveolar nerves) lies lateral to this fold and medial to the ridge produced by the anterior border of the ramus of the mandible; that is the positioning for injection for an inferior alveolar nerve block, commonly used to anaesthetize the ipsi lateral lower enamel and gums. Vascular supply and innervation the cheek receives its arterial blood supply principally from the buccal branch of the maxillary artery, and is innervated by cutaneous branches of the maxillary division of the trigeminal nerve, by way of the zygomatico facial and infraorbital nerves, and by the buccal branch of the mandibu lar division of the trigeminal nerve. Internally, the mucosa of the cheek is tightly adherent to buccinator and is thus stretched when the mouth is opened and wrinkled when closed. Internally, the labial mucosa is smooth and glossy, and reveals small elevations brought on by underlying mucous glands. When the lips are incompetent, the maxillary inci sors will not be so controlled and the lower lip might even lie behind them, thus producing an exaggerated proclination of these teeth. A tight, or overactive, lip musculature may be related to retroclined maxillary incisors. The lips are saved moist each by tongue deposition of saliva and by numerous minor salivary glands within them. These glands are liable to trauma by the tooth, particularly within the decrease lip; this will produce a mucocele as a outcome of both extravasation of saliva into the submucosal tissues or retention of saliva within the gland or its duct. It has a nonkeratinized stratified squamous epithelium, which overlies a loosely fibrous lamina propria, and the submucosa accommodates some fats deposits and collections of minor mucous salivary glands. The oral mucosa masking the alveolar bone � which supports the roots of the tooth � and the necks (cervical region) of the enamel is divided into two main elements. That portion lining the lower a half of the alveolus is loosely attached to the periosteum through a diffuse submucosa and is termed the alveolar mucosa. It is delineated from the masticatory gin gival mucosa, which covers the higher a part of the alveolar bone and the necks of the enamel, by a welldefined junction, the mucogingival junc tion. These color variations relate to differences in the sort of keratinization and the proximity to the floor of underlying small blood vessels, which may generally be seen coursing beneath the alveolar mucosa. Vascular provide and innervation the lips are primarily equipped by the superior and inferior labial branches of the facial artery. The higher lip is innervated by superior labial branches of the infraorbital nerve, and the lower lip is innervated by the psychological department of the mandibular division of the trigeminal. When the tooth occlude, the vestibule is a closed house that only communicates with the oral cavity correct in the retromolar areas behind the last molar tooth on each side. Where the mucosa that covers the alveolus of the jaw is reflected on to the lips and cheeks, a trough or sulcus is shaped, which is identified as the fornix vestibuli. A variable variety of sickleshaped folds containing unfastened connective tissue run throughout the fornix vestibuli. A large frenulum with an attachment near or on the crest could additionally be related to a midline hole (diastema) between the maxil lary first incisors.
Order 2.5 mg altace with mastercard
Cricopharyngeus arises from the aspect of the cricoid cartilage between the attachment of cricothyroid and the articular facet for the inferior thyroid cornu blood pressure time of day 5 mg altace effective. Some authors have described cricopharyngeus as consist ing of a superficial upper oblique portion � the pars indirect � and a lower blood pressure fluctuations altace 10 mg discount with visa, deeper, transverse portion � the pars fundiformis. The upper half attaches to the median raphe while the decrease part forms a round band that lacks a median raphe. Both triangles are postulated to be websites of weak point in the wall of the pharynx and oesophagus, and are due to this fact areas the place diverticula may probably type. Both cricopharyngeus and thyro pharyngeus unfold posteromedially to be a part of the contralateral muscle. Thyropharyngeus is inserted into the median pharyngeal raphe, and its upper fibres ascend obliquely to overlap the middle constrictor; however, cricopharyngeus blends with the round oesophageal fibres around the narrowest a part of the pharynx. This could trap portions (or all) of the passing food bolus, resulting in regurgitation of old meals, aspiration pneumonia, halitosis and weight loss. Treatment could involve open excision or inversion of the pouch to stop it filling, coupled with division of the round fibres of cricopharyngeus, to forestall the buildup of strain within the area and recurrence of the pouch. The plexus lies on the external floor of the pharynx, particularly on the middle con strictor. Filaments from the plexus ascend or descend external to the superior and inferior constrictors earlier than branching throughout the muscular layer and mucosa of the pharynx. The pharyngeal branch of the vagus supplies all of the muscles of the taste bud (excluding tensor veli palatini, which is provided by the mandibular division of the trigeminal through the nerve to medial ptery goid) and all of the muscular tissues of the pharynx (excluding stylopharyngeus, which is equipped by the glossopharyngeal nerve). It emerges from the higher part of the inferior vagal ganglion and consists of axons arising from neuronal cell bodies in the nucleus ambiguus. The nerve passes between the external and inside carotid arteries to reach the upper border of the center pharyngeal constrictor and subsequently divides into quite a few filaments that contribute to the pharyngeal plexus. It also offers off a minute filament, the ramus lingualis vagi, which joins the hypoglossal nerve as it curves round the occipital artery. The plexiform con nections which may be demonstrated between the accessory nerve and the vagus nerve inside the posterior cranial fossa are too variable and insubstantial to assist this operate. The internal laryngeal nerve and laryngeal department of the superior thyroid artery attain the thyrohyoid membrane by passing between the inferior and middle constrictors. The exterior laryngeal nerve descends on the superficial floor of the muscle, just behind its thyroid attachment, and pierces its decrease half. The recurrent laryngeal nerve and the laryngeal department of the inferior thyroid artery ascend deep to its decrease border to enter the larynx. Vascular provide the arterial supply of the inferior constrictor is derived mainly from the pharyngeal department of the ascending pharyn geal artery and the muscular branches of the inferior thyroid artery. Innervation Both parts of the inferior constrictor are usually internal vated by way of the pharyngeal plexus. Although controversial, out there evi dence in humans suggests that cricopharyngeus is also provided by the recurrent laryngeal nerve and the external branch of the superior laryn geal nerve (Sakamoto 2013). Cricopharyngeus is the primary part of the upper oesophageal sphincter, or pharyngooesophageal highpressure zone, the other elements being thyropharyngeus and the proximal cervical oesophagus. Cricopharyngeus accommodates about 40% of endomysial connective tissue, much of which is elastic, but it lacks muscle spindles (Bonning ton et al 1988, Brownlow et al 1989). The tonic exercise of cricopharyngeus between swallows prevents influx of air throughout inspir ation and tracheobronchial aspiration and pharyngeal reflux of oesophageal contents during oesophageal peristalsis. Traditionally described as a reflex, the method is extra properly thought to be a programmed motor behaviour. Swallowing is initiated when meals or liquid stimulates sensory nerves in the oropharynx. In a 24hour interval, a mean particular person will swallow between 600 and 1000 times but, of these, only some 150 will relate to feeding; the rest happen to clear continuously produced saliva and are much less frequent at evening (Sato and Nakashima 2006, 2007). Eating and ingesting are fundamental human pleasures, and issues asso ciated with swallowing can impact dramatically on the quality of life. Swallowing issues are often symptoms of other complex illnesses; an lack of ability to swallow might adversely have an result on nutritional standing and there fore indirectly exacerbate the underlying disease. Aside from the chance of asphyxiation by way of choking, swallowing problems may also be a direct cause of morbidity and mortality as a outcome of aspiration of meals, liquid or presumably refluxed gastric acid contents, inflicting bacterial infection or tissue damage. Swallowing in the adult human has often been studied in relation to swallowing strong or liquid food carried out on command. For descriptive functions, the method has been historically divided into four phases: oral preparatory, oral transit/transfer, pharyngeal and oesophageal (in this conventional view some have solely recognized three phases, combining the two oral phases of preparation and transit right into a single oral phase). Oral and pharyngeal phases Hypopharyngeal diverticula 582 Hypopharyngeal diverticula occur within the lower portion of the pharynx by way of areas of weak point within the pharyngeal wall. The pharyngeal mucosa that lies between cricopharyngeus and thyropharyngeus is rela tively unsupported by pharyngeal muscular tissues and known as the dehiscence of Killian. A delay within the leisure of cricopharyngeus, which may occur anatomy of swallowing (deglutition) overlap when swallowing strong food, however perhaps less so when swal lowing saliva or other liquids. It due to this fact seems applicable to communicate of an oral preparatory and an oral transit section when describing the swallowing of liquids, but inappropriate when contemplating the swal lowing of stable food. Bolus formation appears to contain a number of cycles of transporting meals from the anterior to the posterior a part of the tongue through the palato glossal and palatopharyngeal arches until a bolus accumulates on the oropharyngeal floor of the tongue (retrolingual loading), the val leculae and throughout the oropharynx. Throughout this section, the lateral and rotatory tongue actions that deliver the meals to the teeth for grinding and discount are essential for normal bolus formation as a result of they be positive that the meals is positioned underneath the occlusal surfaces of the tooth. Movements of the tongue are additionally cyclical in phase with the actions of the jaw and hyoid bone. As the jaw is elevated, the tongue is retracted so that it now not lies under the anterior teeth as they as are introduced collectively by jaw elevation. Chewing continues till all the food has been moved posteriorly, a course of that may final from lower than 1 second to as a lot as 10 seconds. The oral preparatory, oral transport and pharyngeal phases of swallow ing subsequently overlap when stable food is being swallowed. The end of this phase of swallow ing is marked by the tongue propelling the prepared bolus of meals to the posterior part of the oral cavity and then on into the oropharynx to provoke the swallow. During swallowing, the muscular tissues that dilate the pharyngotympanic tube are activated during a pause in res piration in the expiratory section. Throughout this primary phase, the soft palate is absolutely lowered by contraction of palatoglossus and palatopha ryngeus, and the posterior a half of the tongue is concurrently elevated; the apposed soft palate and tongue kind a decent seal that helps to forestall premature leakage of the bolus into the oropharynx earlier than the airways are absolutely protected. Slight leakage of fluid does generally occur; the tendency for there to be leakage because of imperfect sealing will increase with age. In the oral transit/transfer section, the liquid in the oral cavity is trans ported by way of the palatoglossal and palatopharyngeal arches into the oropharynx. Genioglossus raises both the tongue tip and the a part of the tongue instantly behind the tip in order that they come into contact with the alveolar ridge.
Altace 5 mg buy visa
The thyroid cartilage develops from the ventral ends of the cartilages of the fourth blood pressure in dogs 5 mg altace order with amex, or fourth and sixth blood pressure medication diuretic altace 10 mg purchase visa, pharyngeal arches. The cartilage appears as two lateral plates, each chondrified from two centres and united in the mid-ventral line by a fibrous membrane, within which a further centre of chondrification develops. The cricoid cartilage arises from two cartilaginous centres, which soon unite ventrally, steadily lengthen, and in the end fuse on the dorsal surface of the tube because the cricoid lamina. Paired arytenoid swellings seem inside the ventral tissue of the sixth arches from stage 14, one on both sides of the cranial finish of the laryngotracheal groove. As they enlarge, they approximate to one another and to the caudal a half of the hypobranchial eminence, the place the epiglottis develops. The opening into the larynx, at first a simple slit, is transformed right into a T-shaped cleft by the enlargement of the arytenoid swellings. The vertical limb of the T lies between the 2 swellings, and its horizontal limb lies between them and the epiglottis. Laryngeal and tracheobronchial veins additionally drain to the precardinal complicated, whilst the capillary plexuses, developed within the (splanchnopleuric) walls of the nice terminal respiratory passages and alveoli, converge on pulmonary veins of increasing calibre, lastly making secondary connections with the left atrium of the center, and could also be grouped with the vitelline systems. The notochordal sheath is wealthy in sulphated glycosaminoglycans, which play a task in inducing condensation and chondrification of the occipital sclerotome-derived mesenchyme around it. Laterally, the exoccipital elements (derived from sclerotomes three and 4) chondrify quickly afterwards; they prolong around the hindbrain to kind the occipital arch, which is developmentally equivalent to the neural arch components of vertebrae. The supraoccipital part of the occipital cartilage extends dorsally from the exoccipital cartilage to full the foramen magnum. After formation of the exoccipital cartilages, differentiation also extends further rostrally in the medial a half of the skull base, with formation of the hypophysial polar cartilages on either side of the hypophysial stalk; they unite in the median plane to form the primordium of the postsphenoid, cradling the hypophysis and retaining a perforation for the hypophysial stalk till the third month. This part of the basisphenoid cartilage will form the sella turcica with its hypophysial fossa. This is the last part of the medial a half of the skull base to differentiate as cartilage, bridging the gap between the postsphenoid and the cartilaginous nasal capsule. At stage 17, mesenchyme begins to condense and later to chondrify around the nasal pits, forming the outer a part of the nasal capsule and the nasal septum; the roof of each nasal capsule is completed slightly later, when cartilage differentiates across the olfactory nerve bundles to kind the cribriform plates of the ethmoid bone. The whole nasal capsule is nicely developed by the tip of the third month, and consists of a typical median septal half, sometimes initially termed the interorbitonasal septum or mesethmoid, and the outer ectethmoid. The conchae ossify in the course of the fifth month; the superior and middle conchae kind part of the ethmoid bone, and the inferior pair turn into separate components. Part of the capsule stays cartilaginous as the septal and alar cartilages of the nostril, and half is replaced by the intramembranous vomer and nasal bones. The most rostral of them turns into steady with the presphenoid cartilage by differentiation of a cartilaginous bridge that varieties the caudal boundary of the optic foramen, enclosing the optic nerve; this later ossifies to kind the lesser wing of the sphenoid bone (orbitosphenoid). The larger wing of the sphenoid (alisphenoid) has both intramembranous and endochondral components; the endochondral half initially differentiates as a cartilage surrounding the mandibular department of the trigeminal nerve, forming the foramen ovale. This condensation extends medially to be a part of the rostral edge of the hypophysial (polar) cartilage on both sides. It additionally extends rostrally to encompass the maxillary branch of the trigeminal nerve, forming the foramen rotundum. Lastly, it extends laterally to be a part of the intramembranous a half of the bone, which replaces the caudal a half of the orbital cartilage. The greater and lesser wings of the sphenoid are separated by the oculomotor, trochlear and abducens nerves and by the first (ophthalmic) division of the trigeminal nerve. The otic capsule differentiates from a mesenchymal condensation across the otocyst, after its morphogenesis to form the cochlea and semicircular canals. Chondrogenesis around the point of exit of the vestibulocochlear nerve creates the interior acoustic meatus. Chondrogenesis of mesenchyme around the carotid arteries joins every hypophysial cartilage to the otic capsule, forming the carotid canals. A gap occupied by the jugular vein and the glossopharyngeal, vagus and accent nerves stays between each otic capsule and the parachordal cartilage; this is the jugular foramen. The neurocranium is composed of the calvaria and basicranium; it surrounds and protects the brain and the special sense organs of olfaction, imaginative and prescient, hearing and stability. The viscerocranium, which incorporates the squamous part of the temporal bone, forms the skeleton of the face, palate and pharynx, and mediates the features of feeding, breathing and facial features; it additionally protects the tongue and varieties the middle ear and the bony exterior acoustic meatus. The boundary between neural crest and cranial mesoderm lies between the frontal and parietal bones (coronal suture) of the calvaria; the skull base is fashioned by neural crest rostral to the tip of the notochord, and is sclerotome-derived. Broadly speaking, the bones of the skull base are shaped by endochondral ossification (chondrocranium), whereas those of the calvaria and face ossify directly from mesenchymal condensations, i. Several bones are of compound construction with respect to their tissue origins and/or sort of ossification: the occipital, temporal and sphenoid bones, and the mandible. Development of the pharyngeal arch-related cartilages of the viscerocranium and ear ossicles has been described within the section on the pharynx. In all of the diagrams, the chondrocranium and cartilaginous stages of vertebrae are proven in blue, except where ossification is happening; right here, the color is green. A, A sagittal part via the cranial finish of the creating axial skeleton in an early human embryo of roughly 10 mm (5 weeks), exhibiting the extent of the notochord. The remnant of the hypophysial stalk is indicated by a black dot within the hypophysial fossa. The strategy of endochondral ossification within the skull is basically the identical as that of the long bones, besides that every ossification centre is equivalent to a major centre, and follows a particular programme of growth and patterning. Growth takes place within the cartilage between adjacent ossification centres; these joints are termed synchondroses. The first ossification centres to appear are these of the lesser and larger wings of the sphenoid, at 8 and 9 weeks, respectively. A single basisphenoid ossification centre appears at 11 weeks; three presphenoid and 4 postsphenoid ossification centres seem at 16 weeks. Bone replaces most of the cartilage until only the most important synchondroses stay; these allow the endochondral skull base and sensory capsules to proceed rising until they reach their ultimate size at puberty or earlier. At delivery, unossified chondrocranium persists within the alae, lateral nasal cartilage and septum of the nose, the sphenoethmoidal junction, the sphenooccipital and sphenopetrous junctions, the apex of the petrous temporal bone (foramen lacerum), and between ossification centres of the sphenoid and occipital bones. In basic, endochondral ossification centres form later than intramembranous ossification sites, which first seem during the seventh and eighth weeks. In humans, as in all mammals, the most important a part of the calvaria is shaped by paired frontal and parietal bones and the unpaired interparietal (membranous part of the occipital bone). The squamous part of the temporal bones and the alisphenoids contribute to the lateral partitions. Lineage information from mouse research indicate that the frontal and squamous temporal bones are of neural crest origin and the parietals are of mesodermal origin; the interparietal is blended (Jiang et al 2002). The coronal suture thus forms on the neural crest�mesoderm interface, as does the sagittal suture, as a result of a small tongue of neural crest tissue lying between the two growing bones. These tissue interfaces are vital for initiating the molecular signalling system that governs growth of the calvaria. In addition to the expansion-related development that takes place within the sutures, appositional growth, during which bone is laid down on, and resorbed from, the bone surfaces, performs an essential function in remodelling the calvarial bones to keep a level of curvature that matches the curved surface of the growing brain. The frontal and parietal bones are initiated as basolateral mesenchymal primordial, which lengthen upwards between the dermal connective tissue and the mesenchymal dura mater. As the frontal after which the parietal primordia extend upwards, the differentiating osteoblasts secrete osteoid, which then undergoes mineralization.